Lipedema Treatment
What is Lipedema?
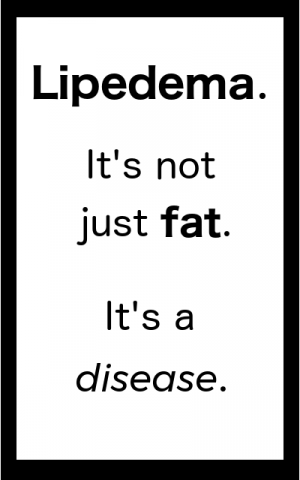
Lipedema is a commonly misdiagnosed fat and connective tissue disorder usually found in women. Lipedema most often affects the legs, is also commonly found on the arms.
It is a progressive disorder which worsens over time. However, there is therapy that can be help ease the symptoms of pain an swelling. Manual Lymphatic Drainage (MLD) along with compression garments and Myofascial Release are the primary modalities used to help this condition. Some people get relief as well through Electro-Lymphatic Therapy (ELT).
Standard of Care
In 2021 many researchers, doctors, and therapists put together a published document in the medical journal Phlebology on the standard of care for lipedema. You can read that document here. If you are looking for information for your physician to help him or her understand the condition better, consider taking a printed copy of this document with you to your next appointment.
Lipedema is a genetic condition and is often triggered by hormonal changes that happen at puberty and menopause/peri-menopause.
Traumatic events such as surgery, especially related to reproductive organs are also suspected as triggers of the disease.
Check out the Lipedema FAQ and Lipedema Resource Pages for more information. Also, the Fat Disorders Research Society has more information on Lipedema.
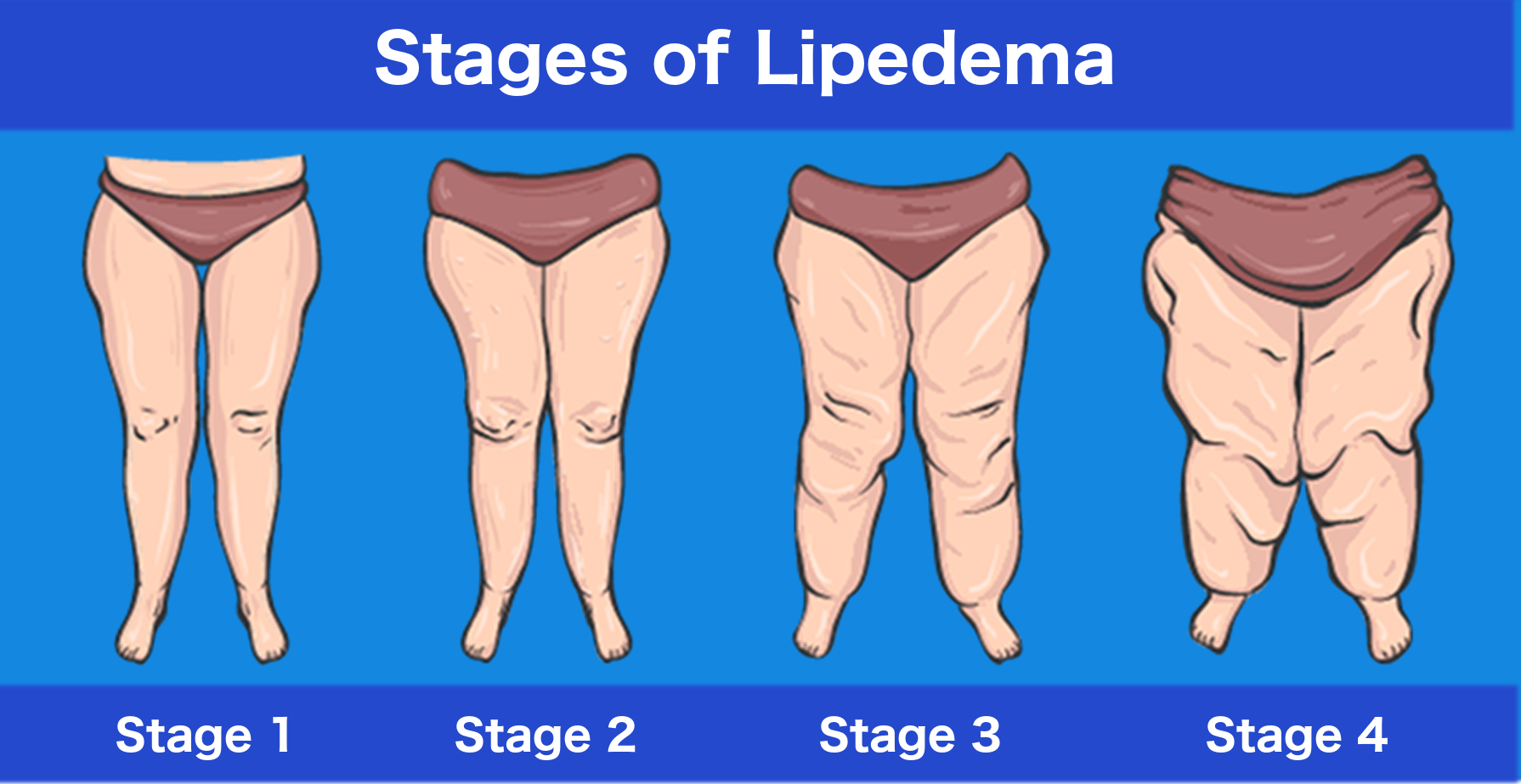
Lipedema has distinct stages which help with diagnosis from a qualified physician.
Learn more about the Stages of Lipedema.
Also of note is that Lipedema is frequently found in people who have
Ehler’s Danlos Syndrome and Mast Cell Activation Syndrome (MCAS/MCAD).
Treatment for Lipedema
1. Lymphatic Massage for Lipedema

Lipedema is greatly aided by lymphatic drainage. Both Electro-Lymphatic Therapy (ELT) and Lymphatic Massage (Manual Lymphatic Drainage (MLD)) are effective in treating Lipedema symptoms.
Lymphatic drainage helps greatly with the extreme sensitivity associated with Lipedema and usually results in a reduction of leg size. However, lymphatic drainage alone is not enough to combat the disease.
2. MYOFASCIAL RELEASE FOR LIPEDEMA

Myofascial Release is the second step in Lipedema treatment.
Once extreme sensitivity has been reduced through lymphatic drainage, a deeper tissue technique known as Myofascial Release is used to break up the adhesion-like fascia and fat cells that are characteristic of Lipedema.
This form of Myofascial Release can start out light, but the goal is to work quite deep into the tissue. Yes, it can be uncomfortable. Yes, people often bruise with this treatment. (Lipedema legs are already prone to easy bruising.)
Most people who have this form of therapy, despite the discomfort, can’t wait until their next session. Why? Because it really helps.
3. COMPRESSION FOR LIPEDEMA
Compression helps many people who have lipedema. The problem is that because most compression is “off the shelf,” meaning it is pre-made for a handful of shapes and sizes, it often doesn’t fit lippy legs and hips.
My personal favorite compression garment for lipedema are Bioflect leggings. Be sure to get the ankle-length variety as the capris tend to dig behind the knee. These are available in numerous sizes, so they probably have one that will fit you. Not wild about the color choices? The tan ones can be dyed with Rit Synthetic dye (done on the stovetop).
Lipedema Treatment Additional Resources
In addition to coming to Pain & Swelling Solutions for your Lipedema Therapy, I highly recommend that you pick up a copy of Lipedema Treatment Guide: A Certified Lymphedema Therapist’s advice for her clients with lipedema. You can get it here on Amazon.
Lipedema Treatment Guide
(amazon link)
The Lipedema Treatment Guide is written by Kathleen Lisson, CLT. She is a colleague of mine, and we have been through much of the same training on lipedema. Her recommendations are in line with the therapies I provide, so I strongly recommend that my clients grab a copy to help them better understand the therapies and strategies I recommend for Lipedema management.
Lipedema Diets
One common question that I get about lipedema is whether or not diet will help. The answer is yes and no. Standard diets (and exercise) DO help regulate regular body fat (not lipedema fat). That being said, fat builds more of itself, regardless of whether it is regular fat or lipedema fat. So, by doing your best to have a healthy diet does help to keep the lipedema fat from becoming worse.
There is only one diet known, however, to reduce lipedema fat directly – and that is the Keto Diet.
Ketogenic Diet
A popular diet known to reduce “Lippy” fat is the ketogenic diet. It does not come without its own risks, however. You should speak with a knowledgeable physician and dietician to determine if this diet is safe for you.
In essence, the ketogenic diet eliminates most carbohydrates from the diet. These carbohydrates are the body’s normal source of energy. In their absence, the body will go into a state known as ketosis which forces it to use fat as fuel. The ketogenic diet has been shown to reduce “Lippy” fat.
Always consult your physician before beginning any new diet.
An Important Word on Keto Diets
Having read a number of books on keto, I would be remiss not to mention that there are some very strange myths and some even worse advice about doing keto. As with many other topics online people who know little to nothing about physiology or nutrition put out fancy-looking infographics that are misleading at best, and dangerous at worst.
Speaking from personal experience, I can state without reservation that being on a keto diet does not require heavy meat consumption (or any at all for that matter). Even if you are vegan you can do keto.
How? It’s about teaching your body to burn FAT, not meat. Plant-based fats can and will put you into ketosis when you limit your carb intake. AND, they are not inflammatory like animal based proteins.
One very good book that speaks to how keto really works is called Unlocking the Keto Code: The Revolutionary New Science of Keto That Offers More Benefits Without Deprivation by Stephen Gundry. While it does not address lipedema, it does talk about how the diet affects your body and how to do it in a safe manner. It also gives some vegetarian and vegan info for people with plant-based diets.
To be successful at a keto diet, one really needs to understand the hows and whys. Dr Gundry does an outstanding job of boiling down several complex topics into everyday language so that they are easy to understand. This understanding makes implementation much easier because it takes out the guesswork.
Unlocking the Keto Code:
The Revolutionary New Science of Keto
That Offers More Benefits Without Deprivation
(amazon link)
Two quick notes about this “diet.” First, it’s not a diet in the common sense of the word. It is a way of eating. Second, you aren’t starving yourself in this “diet” (quite the opposite). You are starving the condition.
In the book, Lymphedema and Lipedema Nutrition Guide: Foods, Vitamins, Minerals, and Supplements, Ehrlic, and others (including the famous Dr. Karen Herbst) describe how to eat to positively impact major lymphatic organs and related processes, including:
- Gut Lymphatics
- Gut Microbes
- Grains and Gluten Metabolism
- The Liver
- The Skin
- Abnormal Biological Signals
- Lipedema Fat
Lymphedema and Lipedema Nutrition Guide
(Amazon Link)
They also describe in great depth the vitamins, minerals and supplements that have a positive impact on both Lipedema and Lymphedema.
This way of eating to starve out Lipedema and Lymphedema is primarily (but not exclusively) a whole foods, plant-based diet tailored to combat these conditions.
The book provides a number of sample recipes, meal plans, a shopping guide, a list of ingredients to avoid, and practical tips such as how to eat when you are not at home.
In the following video, “Eating to Starve Lymphedema & Lipedema” presented at the Lymphatic Education & Research Network (LE&RN) Patient Symposium in 2019, Chuck Ehrlich, MS, MBA discusses how to make dietary modifications to help both Lymphedema and Lipedema.
Lipedema and Exercise
“Lippy” fat is exercise resistant and will not reduce even under the most strenuous exercise programs. Exercise is recommended, however, as it does help to keep the body’s normal fat at normal levels.
While exercising despite the inability to reduce Lipedema fat may seem unimportant, there seems to be a clear link to obesity and the more severe cases of lipedema. Although exercise does not reduce Lipedema fat, it does reduce normal fat elsewhere on the body.
Women who are not obese typically have an easier time keeping the Lipedema from progressing as rapidly. So, keep exercising because it is helping to keep your Lipedema from getting worse faster.
Liposuction for Lipedema
As was mentioned before, Lipedema is a progressive disease, and due to the fact that most women do not get a diagnosis until it is far progressed it often does require specialized liposuction for reduction of the leg size.
The type of liposuction used is referred to as lymph-sparing liposuction because it uses very small tools that do minimal damage so as not to further impair the lymphatic system.

Is Liposuction for Lipedema Covered By Insurance?
Liposuction for Lipedema may be covered by insurance, but it is an uphill battle.
Start by getting a diagnosis from a recommended physician who is familiar with Lipedema.
Document EVERYTHING you are told by EVERYONE. Write out a detailed personal story on how it has affected your life and how having surgery would change your everyday activities.
Expect to be denied. Most women are. Plan on going through an appeal. Expect a fight, but don’t back down.
Find help in support groups on Facebook and other social media sites. There are now certain groups such as Cover Lipedema that help you get all of your paperwork together to submit for insurance coverage and will help you with the appeal process (which is just part of the game you play to get liposuction for lipedema covered).
Don’t give up hope. (Since this page was originally made several years ago a lot has changed, and now many people are beginning to get coverage – sometimes partially, and sometimes in full – for surgery to help remove lipedema fat.)
Lymphatic Drainage combined with Myofascial Release can help reduce the signs and symptoms of lipedema, improve your immune function, and help to keep you healthier.